
How Periodontal Disease Disrupts Daily Blood Sugar Variability: A Study from Okayama University
Understanding the Connection Between Periodontal Disease and Blood Sugar Management
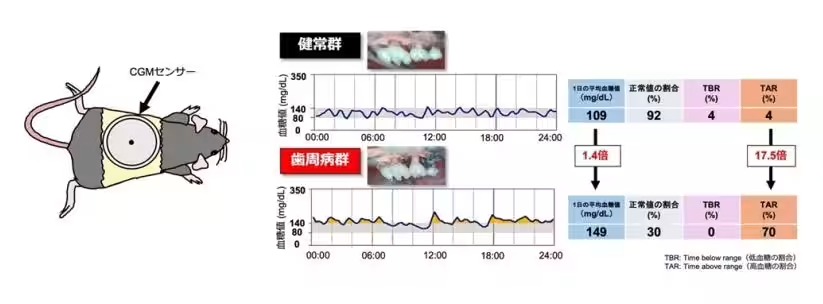
Recent research conducted at Okayama University has unveiled a significant link between periodontal disease and blood sugar fluctuations in diabetes patients. Utilizing continuous glucose monitoring (CGM) sensors on a mouse model with periodontal disease, this study is the first of its kind to confirm how this dental condition can adversely affect blood glucose variability throughout the day.
Research Findings
The research team, consisting of graduate student Moyuka Kubota-Takamori, Associate Professor Kazuhiro Omori, and Professors Masanobu Takashiba and Jun Wada, has highlighted that the inflammation caused by periodontal disease can exacerbate insulin resistance. Additionally, the disturbances in gut microbiota associated with periodontal disease may further deteriorate glucose metabolism. Researchers believe that managing periodontal health could be crucial for diabetes patients not only to maintain stable blood sugar levels but also to prevent complications.
The findings were published on October 6, 2025, in the journal Scientific Reports, making a substantial contribution to our understanding of interconnection within bodily systems.
What Are CGM Sensors and Their Importance?
Traditionally, diabetes management relied on blood tests, including HbA1c and fasting blood sugar readings. However, CGM technology has gained prominence in recent years, allowing for real-time tracking of glucose levels. This innovative approach helps in identifying trends and fluctuations, thus playing a pivotal role in minimizing the risks of diabetes-related complications.
By shedding light on how periodontal disease worsens daily blood sugar variability, this research adds an important layer to the existing knowledge, reinforcing the necessity for a multidisciplinary approach in diabetes care that includes dental health management.
Researchers' Insight
Moyuka Kubota-Takamori shared her experiences about creating the CGM-equipped mouse model, highlighting the importance of monitoring blood sugar variations similar to those seen in humans. She expressed hope that this research will advance collaborative care between medical and dental professionals for better health outcomes in diabetes patients.
Associate Professor Kazuhiro Omori pointed out the unique nature of the study, emphasizing that while there are known correlations between diabetes and periodontal disease, focusing on daily blood sugar changes presents a fresh perspective. He found it particularly intriguing that the inflammation and imbalance of gut bacteria could jointly influence blood sugar levels, indicating vast potential for future clinical studies.
Conclusion
In summary, the study from Okayama University not only uncovers the intricate web of interactions between periodontal disease and diabetes management but also paves the way for further interdisciplinary collaboration. As the understanding of health evolves, it is imperative that dental care becomes integrated into the broader framework of chronic disease management.
For those interested in further information on this groundbreaking study, the research paper titled "Continuous Glucose Monitoring Reveals Periodontitis-Induced Glucose Variability, Insulin Resistance, and Gut Microbiota Dysbiosis in Mice" is accessible through Scientific Reports.
This innovative exploration underlines the significance of maintaining both dental and metabolic health, an essential reminder for healthcare practitioners and patients alike.






Topics Health)










【About Using Articles】
You can freely use the title and article content by linking to the page where the article is posted.
※ Images cannot be used.
【About Links】
Links are free to use.