
Rising Incidence of Physical Restraint in Hospitals Despite Government Efforts
Increasing Incidence of Physical Restraints in Hospitals
A new study conducted by Global Health Consulting Japan (GHC), based in Shinjuku, Tokyo, reveals a troubling trend in hospitals across the country. Despite the government's efforts to suppress the use of physical restraints on patients, nearly 40% of hospitals report an increase in their application. Physically restraining patients—using tools like straps, belts, or administering psychotropic drugs—raises significant ethical questions and poses economic challenges for hospitals. As experts caution, it's crucial for healthcare institutions to understand the reasons behind this increase and work on minimizing the use of restraints to enhance both ethical healthcare delivery and operational efficiency.
Understanding Physical Restraints
Physical restraint refers to the practice of limiting a patient’s freedom of movement through various means, which can involve using physical devices or medications. Generally considered abusive unless justified by emergency circumstances, the use of physical restraints is increasingly scrutinized in light of patient dignity and safety. Recently, there has been a stronger emphasis on establishing standards to ensure appropriate use of these measures.
In the fiscal year 2024, Japan implemented new standards as part of its medical reimbursement framework, mandating hospitals to minimize the application of physical restraints. This includes documentation of the restraint's application during emergencies and the establishment of a dedicated 'Physical Restraint Minimization Team.' Failure to comply with these standards can result in significant financial penalties—essentially deducting 40 points from the daily inpatient fee. In a typical 100-bed ward at a 90% occupancy rate, this could amount to approximately ¥13.2 million in lost revenue annually.
GHC’s Findings
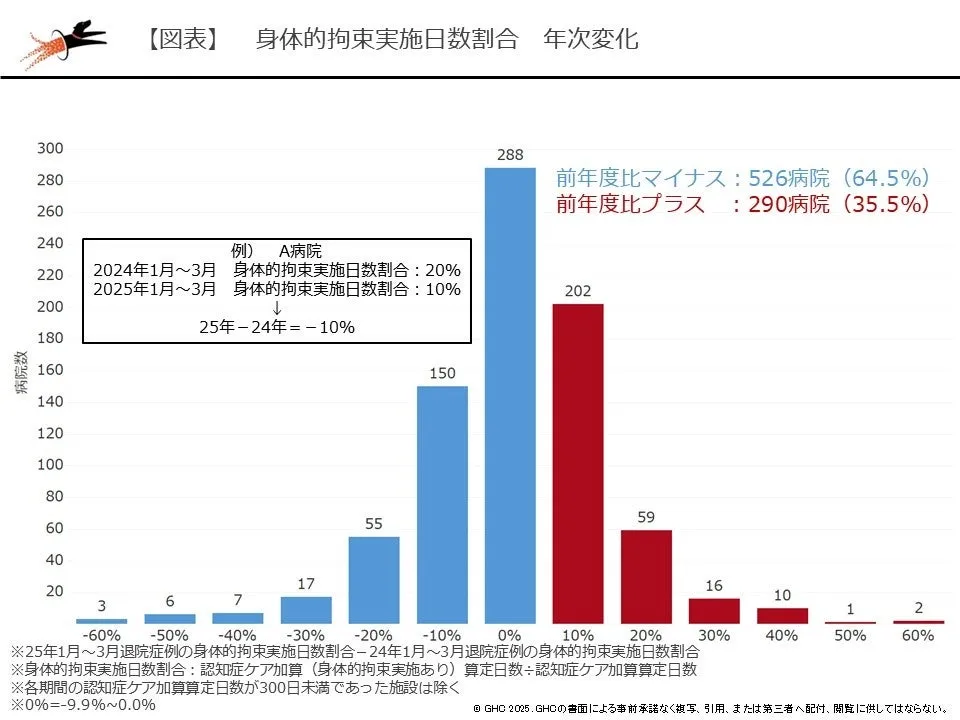
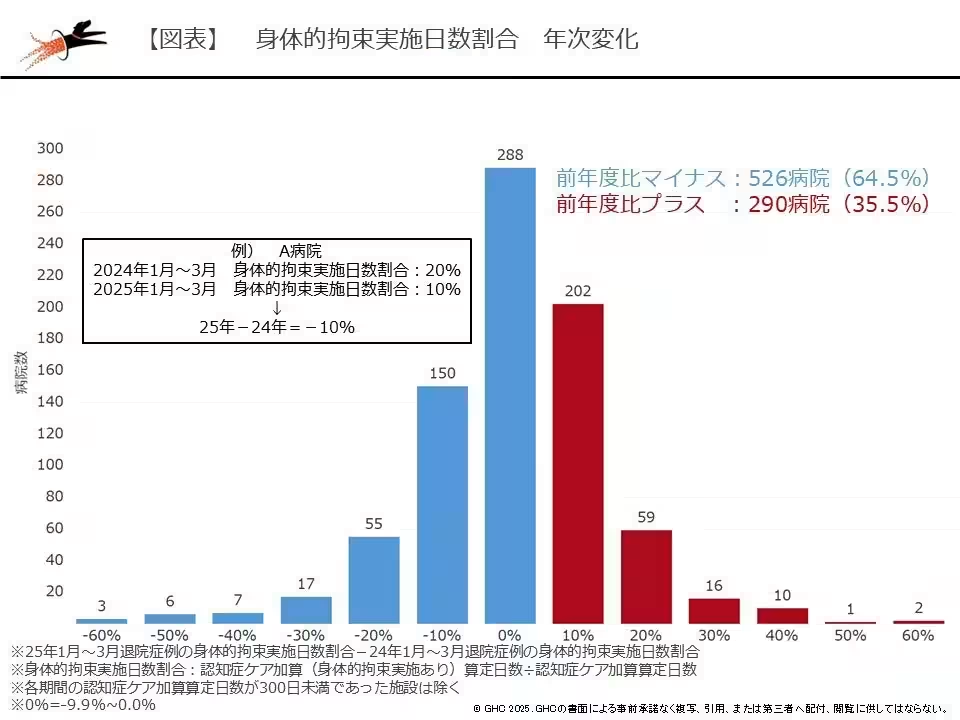
Following the updated reimbursement guidelines, GHC analyzed data from over 816 hospitals to assess how the use of physical restraints has changed. The evaluation focused on periods robustly representative of the healthcare system—January to March 2024 (before the guideline revision) and January to March 2025 (after). The study included 241,941 cases, highlighting the reality of patient care in contemporary Japanese hospitals.
The analysis showed a decrease in the use of physical restraints in 526 hospitals after the new guidelines were implemented, denoted by colored data trends. Conversely, 290 hospitals reported an uptick in restraint use, indicating a disparity in response to the same policy changes.
Consultant Yudai Koiwa, who specializes in physiotherapy and cardiac rehabilitation, remarked, "While progress has been made in minimizing the use of physical restraints, considerable variation exists among hospitals. It's essential to identify the underlying factors contributing to restraint increases in specific institutions. Variables such as an influx of elderly emergency patients or those exhibiting a high risk of delirium may necessitate restraint use, hence sharing these insights within the institution becomes crucial. If the reasons for increased restraint use are unclear, hospitals should revisit their judgment criteria and record-keeping, especially regarding medical interventions that may inadvertently contribute to the need for restraints."
Concluding Thoughts
The tension between patient safety and institutional economic realities highlights the pressing need for a reassessment of policies surrounding physical restraints in hospitals. As the healthcare landscape evolves with demographic shifts and an aging population, understanding the factors driving changes in restraint application will be key to developing responsible, ethical, and effective patient care strategies. GHC remains committed to exploring these dynamics, providing hospitals with data-driven insights to enhance management practices and ultimately improve patient outcomes.
About Global Health Consulting Japan
GHC operates as a consultancy firm specializing in the healthcare sector, drawing on expertise from healthcare professionals, IT specialists, and business management consultants. As the nation faces challenges associated with rapid aging and healthcare funding, GHC focuses on delivering high-quality medical services at optimal costs, pioneering the use of American benchmark analysis techniques in Japan.
Data Analytics in Healthcare
GHC harnesses extensive healthcare big data, including DPC data—a system that consolidates a wide spectrum of medical data. DPC aims to control costs and reduce unnecessary treatments in larger hospitals that serve critically ill patients, making it vital in refining healthcare delivery standards in Japan.
Topics Health)










【About Using Articles】
You can freely use the title and article content by linking to the page where the article is posted.
※ Images cannot be used.
【About Links】
Links are free to use.