
Examining Patient Distribution and Prescription Trends for Diabetes and Chronic Kidney Diseases
Introduction
The healthcare landscape for managing obesity, diabetes, and chronic kidney disease (CKD) is evolving rapidly, significantly influenced by emerging treatment methodologies and prescribed medication patterns. In light of this, Mikcompany Inc., a healthcare data analytics firm based in Tokyo, conducted a comprehensive doctor survey utilizing both an online questionnaire and the SCUEL database to glean insights into the treatment realities and contributing factors impacting these conditions.
Survey Overview
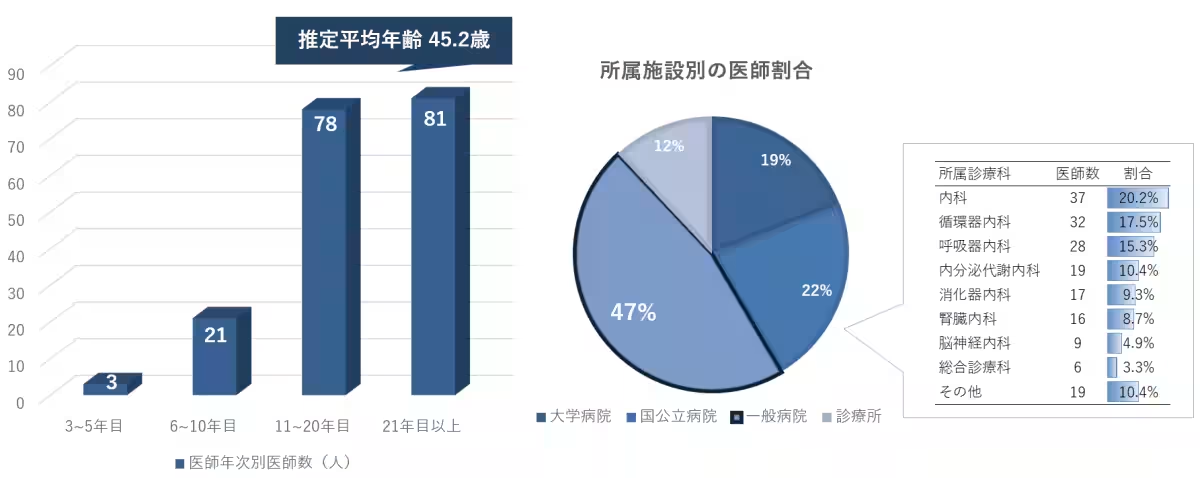
The survey ran from March to April 2025 and involved members of the Antaa Company physician network, yielding 183 valid responses. An impressive 80% of the respondents had over 11 years of experience, indicating a seasoned perspective on the matters at hand. The mean age of the respondents was approximately 45.2 years. Notably, 47% worked in general hospitals, primarily in the departments of internal medicine, cardiology, and respiratory medicine.
Patient Distribution by Specialty
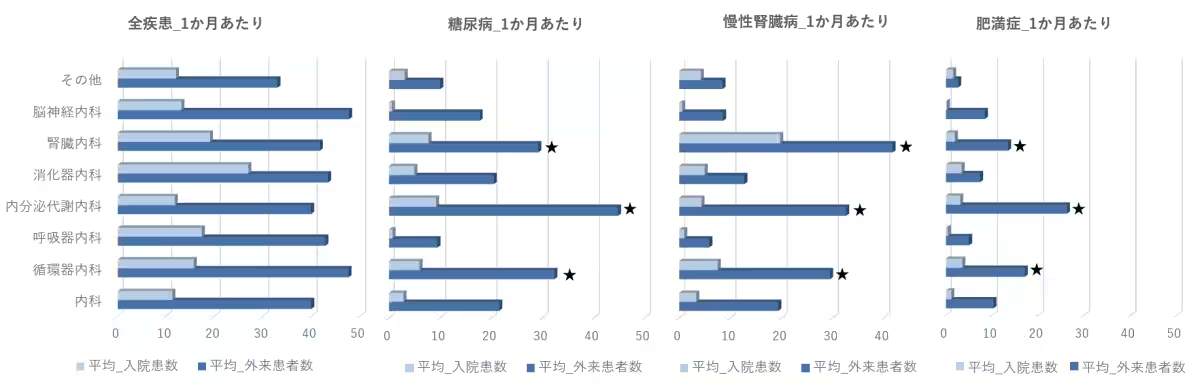
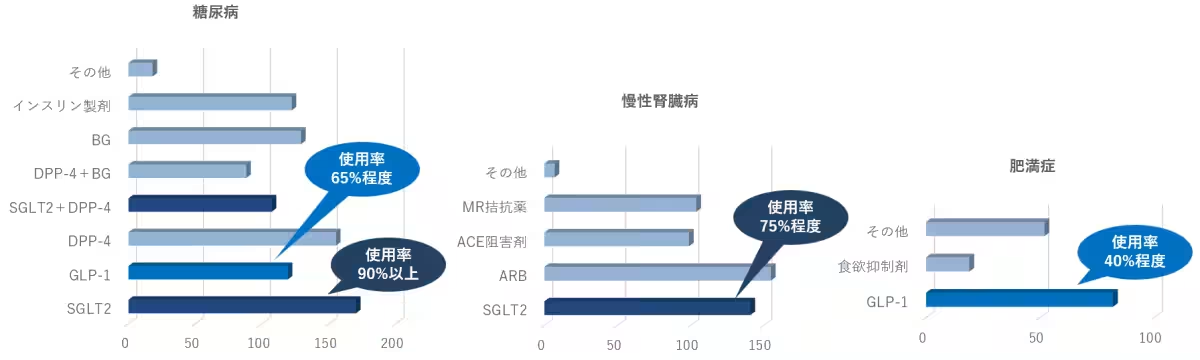
When looking at the distribution of patients treated monthly by specialty, it became evident that endocrinology, nephrology, and cardiology physicians were managing the highest number of cases for diabetes, CKD, and obesity. However, specialized doctors from other fields, including respiratory medicine and neurology, were also treating these conditions, albeit in smaller numbers (about 5-10 patients per month).
The data further revealed that doctors engaged in diabetes management with over 30 outpatients tended to be more likely to be specialists in cardiology, endocrinology, and diabetes management. Conversely, those managing chronic kidney disease cases showed a similar trend toward higher proportions of nephrological and cardiovascular specialists. For obesity cases, there was a notable presence of diabetes specialists.
Prescription Trends Across Conditions
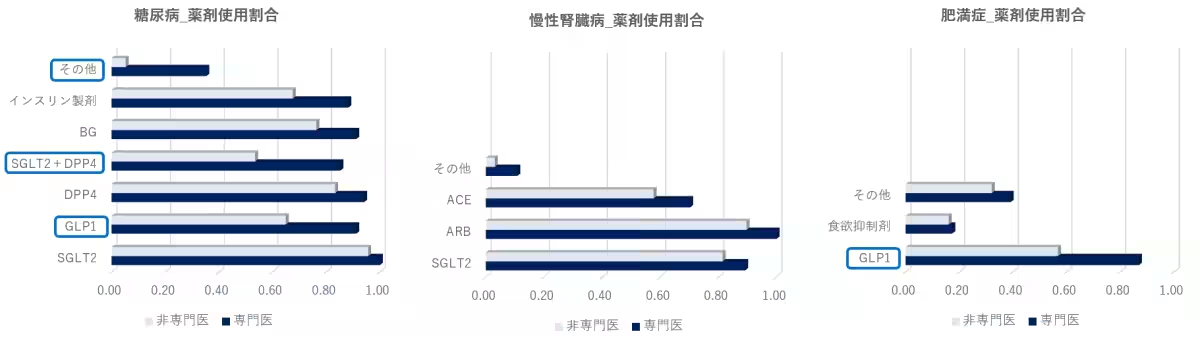
Analyzing the prescribed medications illustrates a clear picture of treatment trends. Physicians treating diabetes commonly prescribed SGLT2 inhibitors and DPP-4 inhibitors, followed by medications such as BG agents, insulin, and GLP-1 receptor agonists. Among the responses for CKD treatment, ARB was the leading choice, followed by SGLT2 inhibitors, MR antagonists, and ACE inhibitors. Notably, GLP-1 receptor agonists were the medication of choice for many obesity specialists.
Statistical data comparing usage patterns across various physicians indicated that doctors who self-identified as specialists in these areas were approximately 30% more likely to prescribe specific treatment options compared to their non-specialist counterparts—especially for GLP-1 receptor agonists and a combination of SGLT2 and DPP-4 inhibitors for diabetes and obesity management.
Decision-Making in Drug Prescription
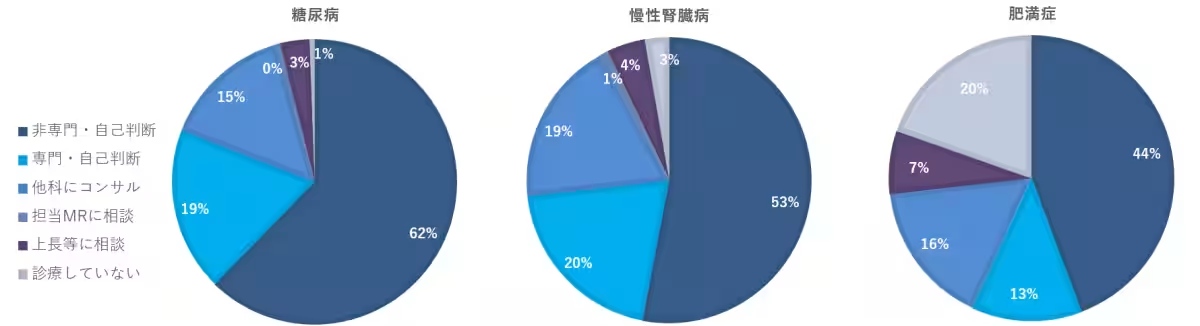
A significant 50% of respondents indicated they made drug choices mainly based on personal judgment, even in areas outside their specialization, with this trend especially pronounced in diabetes care. Only around 20% of doctors acknowledged these conditions as within their specialty, with obesity specialists being even less represented at approximately 13%. A comparable figure of around 20% consulted with superiors or specialists from other fields before making prescriptions.
Conclusion
The intricate dynamics observed in this survey highlight the considerable disparities in both patient management and treatment decisions between specialists and non-specialists in the fields of obesity, diabetes, and CKD. This investigation underscores the importance of ongoing education and collaboration among healthcare professionals to optimize care delivery and improve the quality of patient outcomes. The comprehensive findings can inform future healthcare policies and practices while supporting the ongoing development of medication and treatment guidelines.
For more detailed insights, readers can download our extensive report titled "Realities of Diabetes, CKD, and Obesity Treatment: Results from Antaa Physician Survey" from our website, showcasing a thorough analysis of treatment trends and decision-making in clinical practices.
Topics Health)










【About Using Articles】
You can freely use the title and article content by linking to the page where the article is posted.
※ Images cannot be used.
【About Links】
Links are free to use.