

New Technology Restores Bone Healing Functions Lost with Age Using Drug-Treated Macrophages
Revitalizing Bone Healing for the Elderly
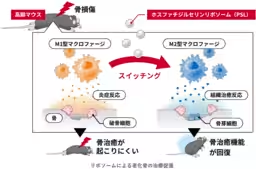
A collaborative effort among top researchers has led to the development of a new technique that addresses the decline in bone healing functions associated with aging. This innovative method involves manipulating the phenotype of immune cells known as macrophages using phosphatidylserine liposomes (PSL). The study demonstrates a significant positive effect on bone healing in aging mice, regardless of their age or sex.
The Importance of Macrophages in Healing
Macrophages are vital immune cells that play a critical role in maintaining tissue homeostasis. They can shift between pro-inflammatory (M1) and anti-inflammatory or healing (M2) phenotypes, which are essential for tissue repair processes. However, aging disrupts this function, delaying the necessary switch from M1 to M2 and impeding the healing process. The researchers discovered that by using PSL, they could effectively encourage this switching mechanism, enhancing bone regeneration in elderly populations.
Clinical Implications
As the global population ages, the incidence of age-related diseases and their associated medical costs are increasing significantly. Hip fractures and other bone injuries in the elderly often lead to prolonged bedridden states, resulting in further complications such as muscle weakness and cognitive decline. The technology's potential to expedite bone healing not only presents a solution to reduce recovery times but could also lower the risk of associated adverse outcomes. This breakthrough signifies a step toward ensuring a healthier, longer life for older individuals, ultimately easing healthcare burdens.
Study Methodology
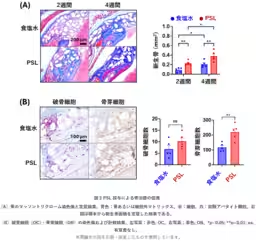
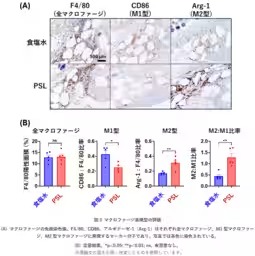
The research, spearheaded by Dr. Chikara Toida from the National Institute of Advanced Industrial Science and Technology, included various experiments to assess the effects of PSL on macrophages. By using male and female mice of different ages, the team analyzed macrophage-derived bone marrow (BMM), identifying significant differences in the secretion of inflammatory factors that characterize M1 macrophages as opposed to their M2 counterparts. Interestingly, while untreated BMMs showed limited inflammatory factor production, the applications of PSL reversed this, indicating successful phenotype switching across different age and sex groups.
Accelerated Bone Healing Results
Further testing involved creating bone defects in the skulls of aging mice and treating them with PSL. Results indicated that PSL administration led to approximately double the speed of bone healing compared to control groups treated with saline solution. This was corroborated by counts of osteoblasts and osteoclasts, showcasing an increase in essential bone-forming cells in the PSL-treated group, alongside a favorable M2-to-M1 ratio, emphasizing the treatment's effectiveness.
Future Directions
The promising outcomes from this study underline the need for continued exploration of PSL in preclinical settings, alongside biological safety assessments to pave the way for practical applications. This could drastically change the landscape for elderly care, providing an essential tool in combating the challenges posed by aging.
This innovation is detailed in the upcoming article in "ACS Applied Materials & Interfaces" scheduled for publication on October 15, 2025, solidifying its significance in the field of regenerative medicine.

Topics Health)






【About Using Articles】
You can freely use the title and article content by linking to the page where the article is posted.
※ Images cannot be used.
【About Links】
Links are free to use.