
Examining Elderly Healthcare Access During the Prolonged Pandemic in Japan
Introduction
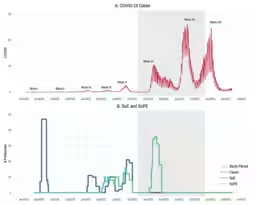
The prolonged COVID-19 pandemic has raised concerns regarding healthcare access among the elderly population. In Japan, where the aging demographic is most prominent globally, understanding the dynamics of healthcare utilization in this context is critical. A recent study led by researchers at Waseda University sheds light on this issue, examining big data from approximately 1.89 million beneficiaries of the late-stage elderly healthcare system.
Key Findings of the Study
The research aimed to analyze whether elderly individuals refrained from seeking medical care during the pandemic's protracted phase. With a data set of about 190 million healthcare claims, the results showed diverse patterns in healthcare utilization:
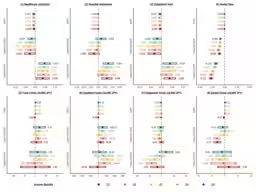
- - Minimal Decrease in Healthcare Visits: Even during the special measures to prevent the spread of the virus, there was only a slight reduction in outpatient visits, by approximately 0.77%. This indicates that, unlike the early stages of the pandemic, the elderly had maintained their access to healthcare services.
- - Daily Medical Expenses Remained Stable: Despite the slight reduction in visits, there were no significant changes in daily healthcare costs. This stability suggests that the types of medical services accessed remained consistent.
- - Equity in Healthcare Access: The study demonstrated minimal disparities in the utilization of medical services based on income, underscoring the effectiveness of Japan's universal healthcare system in ensuring equitable access even during crisis situations.
Disparities in Dental Care Utilization
While general healthcare access remained relatively equitable, noticeable inequalities arose in dental care, particularly among lower-income groups. The data indicated a more pronounced decline in dental check-ups among lower-income elders, highlighting a significant gap in preventative healthcare access.
Importance of This Research
Conducted by a multidisciplinary team from Waseda University, including Associate Professor Fuyou, and researchers Liu Shizhe, Oikawa Masato, Noguichi Haruko, and Kawamura Akira, this study contributes new insights into elderly healthcare utilization during the pandemic's later stages. The experience of Japan can serve as a valuable lesson internationally, particularly regarding healthcare policies in a rapidly aging society.
Implications for Future Healthcare Policies
The findings carry significant implications for public health strategies in face of ongoing crises. Key takeaways include:
- - Preservation of Access to Medical Services: Combining safety protocols with innovative healthcare delivery methods—such as telemedicine—may serve as effective measures to maintain healthcare access during challenging times.
- - Enhancing Monitoring Systems: Establishing systems to monitor the healthcare utilization of vulnerable populations, such as the elderly, children, and disabled individuals, is essential for early identification and risk management in future health crises.
- - Addressing Inequities in Preventative Care: It's vital to ensure that low-income groups have equal access to preventative medical services, including dental care, especially during emergencies.
Conclusion
The ongoing challenges posed by the COVID-19 pandemic have underscored the need for robust healthcare systems capable of adapting to crises. Japan's universal healthcare structure has demonstrated resilience in maintaining access, but the disparities observed in dental healthcare utilization reveal areas needing urgent attention. Harnessing the lessons from this pandemic will be crucial in strengthening the healthcare system for future public health emergencies. By addressing social inequities and enhancing service accessibility, we can better prepare our society for the health challenges that lie ahead.
Topics Health)










【About Using Articles】
You can freely use the title and article content by linking to the page where the article is posted.
※ Images cannot be used.
【About Links】
Links are free to use.